NON-MELANOMA SKIN CANCER
 Overview
Overview
Skin cancer is the most common of all cancers. Reducing exposure to ultraviolet light from sun’s radiation can prevent most skin cancers. Skin cancer if detected early is treatable.
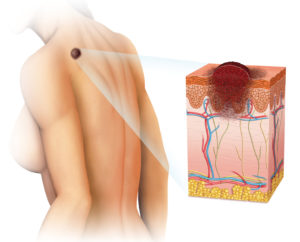
The skin, the body’s largest organ protects against infection and injury and helps regulate body temperature. The skin also stores water and fat and produces vitamin D. Skin is made up of two main layers. The epidermis (outer layer of the skin) and the dermis (inner layer of the skin).
Types of Skin Cancers
There are three main types of skin cancers
Squamous cell carcinoma – Most of the epidermis is made up of flat, scale like cells squamous cells. Cancer of these cells is called Squamous cell carcinoma. It usually arises from sun exposure, but can appear on skin that has been burned, damaged by chemicals, or exposed to x-rays.
Basal cell carcinomas – Cells in the lower epidermis are round cells known as basal cells. A great majority of skin cancers develop from this type of cells that have been exposed to the sun and is called basal cell carcinoma. Basal cell carcinoma most often forms on the head & neck.
Melanoma – Where the epidermis meets the dermis, there are scattered cells called melanocytes, which produces, the melanin that gives skin color. Melanoma starts in melanocytes, and it is the most serious of the three cancer types.
Squamous cell carcinoma and basal cell carcinoma are known as non-melanoma skin cancers.
Risk Factors
Exposure to UV Radiation.
Fair Skin – Less pigment in skin means poorer protection against UV radiation. Those who burn easily by exposure to sunlight are more likely to develop skin cancer.
Gender – Rate of skin cancer in white people has increased in recent years.
Age – Most basal cell and Squamous cell cancers appear after age 50, but may appear earlier in individual with sun-damaged skin.
Individual History – People with weakened immune system or those who use certain medications such as immunosuppressive drugs, certain steroids and drugs that makes the skin sensitive to light, are at a higher risk for developing skin cancer, particularly Squamous cell cancers.
Precancerous condition – Two types of lesions known as actinic keratoses, characterized by rough, red or scaly skin, or Brown’s disease which is common in people exposed to sun. Such conditions can lead to Squamous cell cancers.
Viral infections – People infected with a specific type of Human Papiloma Virus (HPV) are at increased risk for developing Squamous cell carcinoma, particularly if their immune system becomes suppressed.
Signs & Symptoms of non-melanoma skin cancers
An open sore that bleeds, oozes, or crusts, and remains open for several weeks.
A Reddish raised patch, or irritated area that may crust or itch, and rarely hurts.
A shiny pink, red or white pearly or translucent bump.
A pink growth with an elevated border and crusted central indentation.
A scar-like, white yellow or waxy area, often poorly defined.
An elevated growth with a rough surface and a central depression.
Diagnosis as per modern science
Skin biopsy
Shave biopsy
Punch biopsy
Incisional and excisional biopsy
Lymph node biopsy
Fine needle aspiration biopsy
Surgical lymph node biopsy
Staging
Stage 0 – Squamous cell carcinoma in situ, also called Bowen’s disease.
Stage I – The cancer is small and has not spread to lymph nodes or other organs.
Stage II – The cancer is large and has not spread to lymph nodes or other organs.
Stage III – The cancer has spread to tissues beneath the skin, such as muscles, bones, or cartilage, and or it has spread to regional lymph nodes.
Stage IV – The cancer is very large size, and it has spread to lymph nodes. It has spread to other organs such as the lungs or brain.
MELANOMA SKIN CANCERS
Overview
Melanoma is a cancer that begins in the melanocytes. Because most melanoma cells keep producing melanin, melanoma tumors are usually, but not as a rule, brown or black. Melanoma is much less common than basal cell and Squamous cell skin cancers, but it is very difficult to cure.
Melanoma mostly appears in fair skinned people, but colored skin people are also affected. This cancer can develop on the palms of hands, soles of feet, and under the nails. Rarely, melanomas can form in the inner parts of the body, like eyes, mouth, vagina, and other internal organs.
A kind of skin cancer that looks like melanoma is called spitz nevus. These tumors can be mistaken with melanoma. These are generally benign and do not spread, but sometimes diagnosis is difficult to differentiate between the two.
Risk Factors
Moles – A nevus is a benign tumor. Moles are not usually present at birth but begin to appear in children and teenagers. Having certain types of moles makes a person more likely to develop melanoma.
Having a dysplastic nevus or atypical mole, increases a person’s risk of melanoma. Dysplastic nevi, looks like normal moles, but may typically look a little like melanoma. They can appear in areas that are exposed to the sun, as well as those areas that are usually covered, such as the buttocks and scalp. They are larger than moles.
Fair skin – The risk of melanoma is very high, almost 20 times in white skin people as compared to colored skin people. The skin pigment has a protective effect. Each person regardless of skin color can develop melanoma, particularly on the palms of the hands, on the soles of the feet, under the nails, inside the mouth, and rarely in internal organs.
Family history – Risk of melanoma is higher if a member of the family has had the disease.
Immune suppression – People who have been treated with medicines that suppress the immune system, such as organ transplant patients have an increased risk of developing melanoma.
Exposure to Ultraviolet light radiation.
Age – The risk of melanoma increases with age.
Signs & Symptoms
One half of the mole does not match the other half.
The edges of the moles are irregular, rugged, blurred or notched.
Color over the mole is not the same. There may be different shades of tan, brown or black, and sometimes patches of red, blue or white.
The mole is large in diameter. Usually 3 to 6 millimeters in diameter.
Diagnosis as per modern science
Incisional and excisional biopsy
Shave biopsy
Punch biopsy
Staging
Stage 0 – The melanoma in situ, it involves the epidermis but has not spread to the dermis.
Stage I – The melanoma is less than 1.0mm in thickness, and is not ulcerated. It appears to be localized in the skin and has not spread to the lymph nodes or distant organs.
Stage II – The melanoma is between 1 to 4 mm in thickness and is ulcerated. It appears to be localized in the skin, has not spread to lymph nodes or distant organs.
Stage III – The melanoma has spread to lymph nodes near the affected skin area. There is no distant spread.
Stage IV – The melanoma has spread beyond the original area of the skin and nearby lymph nodes to other organs, such as the lungs, liver or brain, or to distant areas of the skin or lymph nodes.

 Overview
Overview